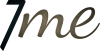
Te Whatu Ora Health NZ has ordered all districts to book appointments for patients on surgical wait lists. Photo / Michael Cunningham
Northlanders waiting for more than a year for surgery could soon get their first hospital appointment after new health authority Te Whatu Ora Health NZ ordered all regions and districts to actively tackle their backlog.
As part of the planned care taskforce Health Minister Andrew Little announced in May, Te Whatu Ora has asked hospitals to book appointments for patients who have been waiting more than 12 months. The deadline is August 31.
Patients waiting for their first specialist assessment for more than 12 months need to be booked for an appointment by September 30.
When the taskforce was announced in May, 3549 Northlanders were waiting for an operation. It is not clear how many of those have been waiting more than 12 months.
Te Whatu Ora Te Tai Tokerau will only release current data under the Official Information Act, which the Northern Advocate has actioned.
Nationwide, 7475 patients are waiting longer than 12 months for treatment and 4073 patients are waiting longer than 12 months for their first specialist assessment.
In an interview with RNZ, Te Whatu Ora chief executive Margie Apa was asked if the deadline was realistic.
“We’ll find out when the districts and regions come back to us and tell us what’s impossible.
“It is important to note that the direction was to book and as part of booking every service should be looking at the waitlist, including assessing if people still needed the appointment or the procedure.”
Apa told RNZ she didn’t know yet how far out these appointments would be. Realistically, it would still be months or more than a year until patients will see a specialist or get their surgery.
Some patients will likely travel to other regions for an appointment if those areas have more vacancies than their local hospital.
Apa admitted there was a chance hospitals won’t be able to deliver on those appointments as hospitals are “pretty full” but New Zealanders had waited too long so action must be taken.
Te Whatu Ora was looking at understanding what capacity hospitals had and what was achievable.
Efforts to hire new staff were ongoing but “we’re not going to be able to magic up theatres and clinical spaces”.
She said the point of the directive was to assess the situation in a nationally consistent way and to ensure “that we’re all working to the same timeline”.
“We have accepted that we don’t have enough resources within the public system now,” Apa said but the taskforce would look to work more closely with the private sector to expand the capacity.
The taskforce is also looking at how general practices can help tackle the current backlog. GPs will be asked to help with assessments and diagnostics.
“Planning is under way to increase the amount of care provided to people by general practitioners, nurses and allied health professionals and look at the resources required to do this.
“This would release senior medical officers working in hospitals and specialist services to provide care others cannot,” a Te Whatu Ora spokesperson explained.
It was not the authority’s intention to replace health professionals with a non-clinical workforce.
“Some of the plans being developed do seek to engage highly skilled clinical workforces, such as nurses and allied health professionals, to carry out tasks they currently might not”