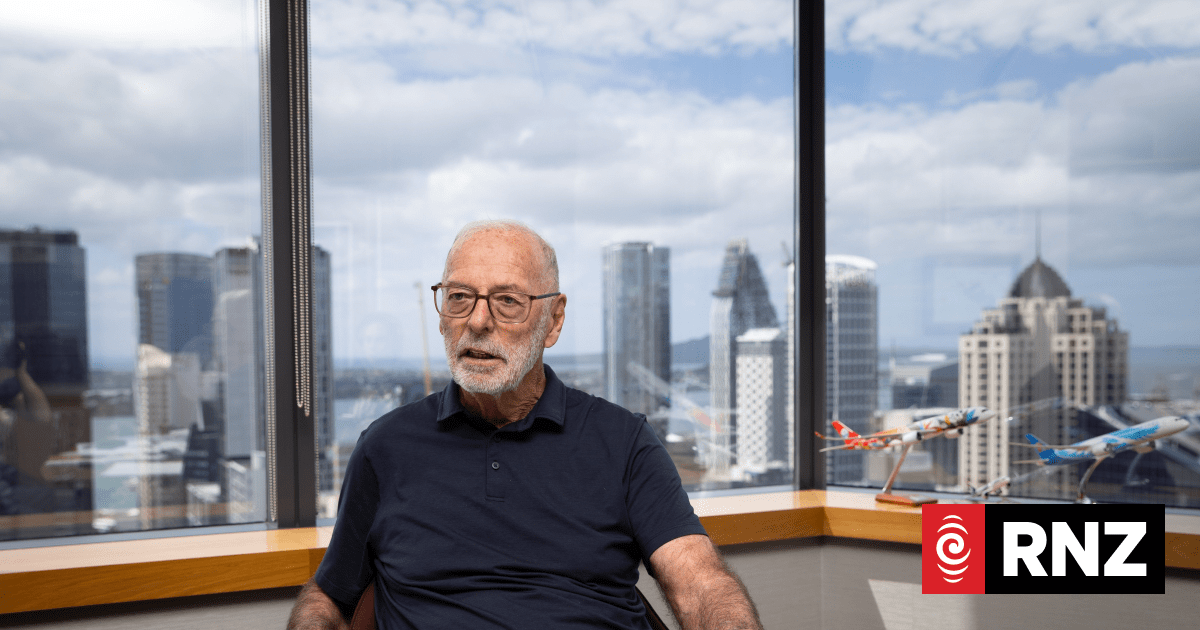
Genevieve Mora says the health sector is under-resourced when it comes to eating disorders. Photo / Supplied
The rise in people suffering from eating disorders has hit crisis point in recent years, and it’s expected with the Christmas period approaching, the stress and anxiety associated may have further impact.
Eating disorders are
most common among children and adolescents, data shows, and often families and friends of those suffering feel helpless as their loved one waits for clinical help.
Genevieve Mora, co-founder of mental health charity ‘Voices of Hope’, says eating disorders can become ”all consuming for everyone in their support network.”
Mora, who has been very open about her mental health journey, told the Advocate her story.
“I spent a lot of my teenage years very unwell and felt a lot of shame,” she said.
Mora struggled with anorexia nervosa, obsessive compulsive disorder and anxiety that led to many visits to the hospital.
“I never set out wanting to change my appearance, for me it was the overwhelming anxiety and a feeling that I had no control over my life.”
Managing her food intake gave Mora a ‘sense of control’, but she quickly discovered she wasn’t in control at all.
“It’s hard for people on the outside to understand,” she said, “and there’s a lot of misconceptions, so advocating in the eating disorder space has become really important to me”.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/CYLFKWWRYV5YDG3VZIGU5P46X4.jpg)
Parents and caregivers often bear the heavy weight of trying to take care of someone who is very unwell, and are unsure of what to do. So what are the options?
Kirsty Ross, clinical psychologist and senior lecturer at Massey University, told the Advocate there are many ways to support those suffering with eating disorders, and also for carers to support themselves.
It is important for a person with an eating disorder to stay in contact with their GP.
“GP involvement is really important, both as that referral pathway but also making sure people are medically safe,” she said.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/E7S77GE7LSDMMV3O4EJDQSDXZA.jpg)
Ross has 20 years of clinical experience, and holds a “trauma informed, strengths-based and recovery oriented perspective”.
She is also someone who experienced an eating disorder as a teen.
Ross said eating disorders can often trigger tension within families, something that needs to be managed.
“For someone who hasn’t experienced it, the level of distress around eating, and food, is really hard to understand.”
She reminded people that statements such as ‘eat a pie’ are unhelpful, and the stigma associated with weight gain places a lot of shame upon those who struggle with over-eating.
“It’s important to remember that it’s a symptom of distress rather than it being attributed to some kind of personality characteristic.”
Ross said validating and collaborating with the person suffering is a great way to tackle the issue.
This includes asking ”what can I do to help?” and ”what can I do to support you?”.
“Often people can go to solutions,” she said.
”But instead of just rushing in to tell someone what they should do, just recognise that this is something more complex and deep. Just accept how it is for that person, that’s not condoning it, but validating the emotion.”
Ross also acknowledged that watching a loved one go through an eating disorder can be ”really distressing”.
“Particularly when it’s a younger person, part of how we show love for someone is through nourishing them,” she said.
For those struggling with under-eating, she said parents should try to remember “it’s not a rejection”.
“It’s important to see the problem as the problem, and the problem is the eating distress.
“It’s okay to have some boundaries as well.
“It’s okay to say ‘I really want to work with you but a bottom line needs to be put there’ to maintain someone’s safety.”
She also reminded people that self care is important, which also means, “having a good cry with a friend, getting good sleep, nourishing your body and moving your body”.
Mora said in her advocacy work she talks to a lot of parents who feel “helpless.”
“I think the best thing to do is show them (those suffering) that you believe in them.”
For 15 to 24-year-olds, the year of 2014 saw 91 cases of eating disorders resulting in hospital admission, whereas in 2020, 241 hospital admissions took place.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/GVRV6PBKZPNCR2AO6TPQLPUFIQ.jpg)
While the number of cases increased significantly, the funding has not.
Mora said while she was fortunate enough to be in a position where her parents could avoid care for her, many are not, which she finds “heartbreaking.”
“Asking for help can be one of the hardest things to do,” she said, “and to be told you’re not sick enough or that you’re going to be put on a waitlist is really invalidating”.
“Not getting immediate support isn’t a reflection of how sick you are, it’s a reflection of how broken the system is,” she added.
Mora believes the issue lies with funding.
“It’s a really under-resourced sector when it comes to funding. Services are really overwhelmed… and more needs to be done about that.”
She also suggested more support is needed for GPs.
Mora often encounters people in the sector who are “just as frustrated and heartbroken as we are as the people trying to get support”.
“Services like Eating Disorder New Zealand support hundreds of families and they’re not funded at all.
”With the significant increase (in those suffering) and minimal funding boost, more needs to be done.”
According to Dr Odette Miller, the average wait time for eating disorder referrals in Northland is 14.9 days since the start of 2020.
Miller is the service manager for the Infant, Child, Youth, Maternal Mental Health and Addiction Services and Early Intervention Psychosis Service for Te Whatu Ora Te Tai Tokerau.
During the Covid-19 pandemic, increases in eating disorders were due to the challenging circumstances that families were living in, coupled with financial uncertainty and isolation from peers, she said.
“For those experiencing these issues, we know that controlling or restricting eating is one of the ways people feel that they can maintain a sense of control, when their world feels unsettled.”
This year, the Northland wait time for eating disorder referrals has reduced to an average of 11 days.
“Within Te Roopu Kimiora (Child and Adolescent Mental Health & Addictions Services), we have access to an Eating Disorders Specialist Clinic for young people and their families, provided at the Whangārei site and there are telehealth appointments available across Northland via this clinic.”
This help is led by a doctor with specialist eating disorder experience as well as social workers and nurses.
“If you have any concerns please seek the support of your GP, even if you feel that you don’t need a referral to Te Roopu Kimiora, keeping your GP informed means there is ongoing medical monitoring,” she said.
Young people and their families are able to self-refer to Te Roopu Kimiora access the service via their GP.
“Once a referral is sent, we will ascertain how quickly a young person needs to be seen and whether any tests need to be completed,” Miller said.
please sidebar or fbox in print Help for parents and caregivers:
EDANZ – improving outcomes for people with eating disorders and their families. Freephone 0800 2 EDANZ or 0800 233 269, or in Auckland 09 522 2679. Or email info@ed.org.nz.
Parent Help – 0800 568 856 for parents/whānau seeking support, advice and practical strategies on all parenting concerns. Anonymous, non-judgemental and confidential.
Family Services 211 Helpline – 0800 211 211 for help finding (and direct transfer to) community based health and social support services in your area.
If you know someone with an eating disorder, or are struggling with one yourself, you can reach out to the following places:
Eating Disorder New Zealand 0800 2 EDANZ Youthline- 0800 376 633 What’s Up (for 5-18 year olds)- 0800 942 8787 thelowdown.co.nz or free text 5626 Healthline- 0800 611 116 Voices of Hope- www.thevoicesofhope.org/resources-index Love your Kite – An App resource to support Eating Disorder Recovery- www.loveyourkite.com