Over three months, National’s health spokesperson shadowed medics after hours around the country. He tells investigations editor Alex Spence it confirmed his belief our emergency medical system is at a critical point.
One night last
month, Dr Shane Reti’s phone was lighting up with messages from contacts at Waikato Hospital, where the emergency department was even busier than usual.
“Truly shocking,” one staffer told National’s health spokesperson. “Staff under extreme pressure and a tsunami of patients. Nowhere for them to be seen and no beds in wards for them either.”
“Expecting someone to die here today,” said another.
Reti – the MP for Northland, a practising GP and the likely health minister if the National Party returns to government after October’s general election – was already particularly concerned about overcrowding at Waikato’s ED. He had seen it himself in early March.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/OBZVQ353LZHPBANPQFHJ5F2OKE.jpg)
Between Waitangi Day and Easter, Reti says he went on 19 night shifts with Hato Hone St John Ambulance crews to get a close-up look at our embattled after-hours acute medical services.
“I wanted to see what the after-hours provision was like,” Reti says. In three months, he shadowed ambulance crews in almost all of the former district health board territories, which took him inside almost all of the country’s emergency departments at some of their busiest times. Te Whatu Ora – Health New Zealand, the national health organisation that operates the public hospitals, says it did not know Reti was coming.
The exercise confirmed his belief that our acute medical system, and particularly hospital EDs, are reaching a critical point, Reti says.
Advertisement
“I’ve been saying for ages, our health system is gonna break at some point,” Reti told the Herald in an exclusive interview. “There are two areas [in which it’s] going to break: EDs and aged residential care. Those are the ones that are hurting the most.”
Overcrowded EDs are an indicator of stress in the wider health system, experts say, reflecting not just the treatment available for the acutely unwell but problems in primary care and hospital services upstream. This month, an investigation by the Herald revealed EDs across the country are facing unprecedented strain in the aftermath of Covid-19.
The pandemic compounded systemic problems created by years of poor planning and under-investment by successive governments – including those led by Reti’s party – leaving hospitals desperately short of experienced doctors, nurses and other staff to care for the acutely unwell.
Staff are burned out, demoralised and increasingly worried about the safety and quality of care they are able to provide their patients, our investigation revealed. In an exclusive interview, a senior doctor said she is so concerned about working conditions at Auckland City Hospital that she is considering quitting emergency medicine.
This week, Te Whatu Ora published updated data on several key national health metrics showing that the number of people presenting to EDs nationally in the first three months of this year has increased 9 per cent compared to the same period last year.
Several EDs experienced double-digit increases. Canterbury and Waikato were the busiest, with each receiving an average of more than 300 patients a day.
The percentage of patients waiting long periods in EDs has also increased, the data shows.
In the greater Wellington region, for example, the percentage of patients waiting more than six hours to be seen increased from 33 per cent to 51 per cent in a year.
Advertisement
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/N7ZJQ6ICDRAWDEATZWWFS7ZUYU.jpg)
“Emergency departments have been under consistent pressure, with increased numbers of people presenting since the pandemic,” Health Minister Dr Ayesha Verrall told the Herald.
Verrall says the acute medicine system has been one of her top priorities since she replaced Andrew Little as health minister in February, and the Government is taking several steps to improve it.
These include introducing a winter preparedness plan that resources pharmacies and other community services to relieve pressures on hospitals, and the launch this month of a plan to recruit and train more frontline staff.
In an exclusive interview, Verrall said that staffing has improved in EDs in the past year because Te Whatu Ora has recruited more nurses.
A senior doctor in one of the busiest EDs says this has not relieved the pressures at their hospital because the new recruits are inexperienced, senior nurses are leaving, shortages of doctors have worsened and workloads have increased.
“I’m not going to argue with you that there are still staffing pressures,” Verrall said. “And that’s why we presented a comprehensive plan.”
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/CVTBRCWL55BRTOF4UITJ7BKHPA.jpg)
The Government is also committed to putting more investment into primary care services so that more people can get treatment at home or in the community without needing to go to hospital, Verrall says.
Reti – who could be responsible for this crisis in less than four months if National forms a government after October’s election – says he shares the frontline clinicians’ concerns.
“There are red flags popping up around the system,” he says.
Reti would say this: he is an opposition politician campaigning in an election year. But his criticisms, Reti says, are supported by what he has recently seen first-hand in dozens of hours with after-hours medical teams.
Hato Hone St John Ambulance allowed Reti to accompany ambulance crews as an observer on 17 occasions, the service confirmed. Reti did two more with Wellington Free Ambulance.
Reti says he witnessed a wide range of medical problems with the ambulance crews, including wounds from assaults, drug overdoses, fractures, respiratory illnesses and psychiatric emergencies.
Reti says the experience confirmed his impression that acute medical services are under extraordinary pressure – and that Waikato Hospital stood out as the busiest.
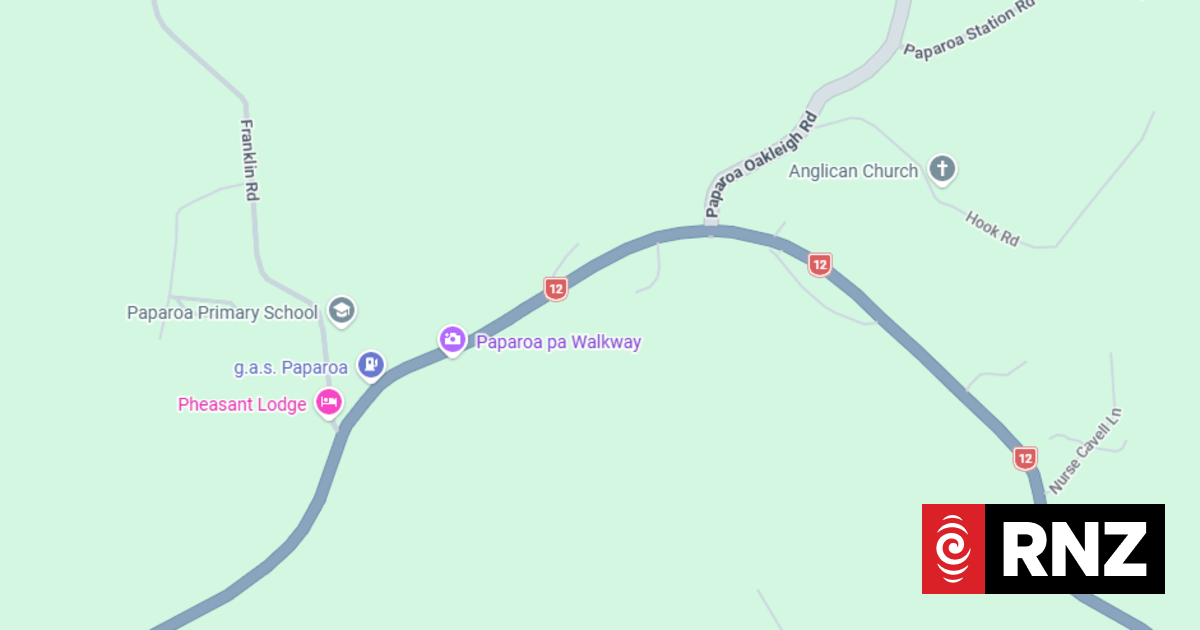
On the night in March that he spent in Waikato, there were only 10 ambulances covering a region from Mercer to Taupō, and they were overwhelmed. At one point, he says, half of the ambulances, including his, were stuck outside Waikato Hospital ED waiting to offload patients – an event known as “ramping”.
Hato Hone St John said it had five ambulances ramped that night between 8pm and 9pm, which amounted to a total of nine hours of waiting.
Inside the hospital, Reti says the waiting room was overflowing and nurses were struggling to stay on top of the situation.
“I did my clinical time in Middlemore,” Reti says, “so I know what a busy ED is like. I have never seen an ED that busy. I was shocked.”
Reti’s ambulance was transporting a woman who had suffered a major fracture and lay on a cold floor for a long period because the paramedics were too busy to reach her sooner. She wasn’t at imminent risk of death, Reti says, but she needed treatment.
He says they waited more than an hour before the woman could be offloaded and the ambulance could return to duty.
On June 27, after Reti received the panicked messages from his contacts at the hospital, he wrote to Verrall asking her to urgently look into “significant concerns for overloaded staff and patient safety at Waikato ED”.
Verrall replied two days later saying Waikato ED had 274 patients that night and the hospital was short of beds. The hospital implemented “escalation pathways” in response to the influx, redirecting non-urgent patients to other clinics and deploying staff from other departments to support the ED.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/J34CMNSABRKY4535ADM4EPWEJI.jpg)
Te Whatu Ora said it could not confirm Reti had visited its EDs with the ambulance crews because it had not been informed he was coming, though it did not dispute that he had done so.
Te Whatu Ora said it was “generally accepted practice” when an MP goes to one of its facilities that it is made aware of their plans, for safety and privacy reasons, and it has “reset expectations with providers” and is putting “clearer procedures in place” for future visits by politicians.
In Reti’s view, one of the main reasons for the pressures on EDs is the deficiencies in primary care.
A high proportion of patients on the callouts Reti observed did not need hospital treatment, but in many places there either wasn’t a GP or the local primary care providers did not have the staff to offer a late-night service.
“There’s just not enough of them,” Reti says. “They’re so exhausted with what they’re doing during the day, it’s really hard to lay an after-hours tier on that.”
So what would Reti do to resolve the pressures on acute care if he becomes health minister?
First, he says ministers have to acknowledge that the system is in crisis. “By at least acknowledging this is a health crisis, it does several things. First of all, it shows that you’re in touch. And secondly, it attracts resources and funding.”
Reti says the system could use the resources it already has more efficiently – for example, by adopting app-based services that would tell patients where to go for the quickest access to treatment. People sometimes end up waiting for hours at a busy public hospital for non-critical problems when there are clinics in the community that could see them much quicker, he says.
And Reti says he would reintroduce the targets for ED waiting times that Labour scrapped against the objection of some senior doctors.
“Targets save lives,” Reti says.
In the longer term, he says, there will need to be a sustained, comprehensive effort to increase the medical workforce.
National has promised to pay a portion of nurses’ student loans if they agree to stay in the sector for at least five years, and pledged to introduce six-month visas and relocation grants to lure more foreign nurses here. And last week, it announced it would build a new medical school in Waikato to train more doctors.
Among frontline staff, there is scepticism both that National’s policies would make a significant difference and that the party is committed to long-term transformation.
Reti admits that previous National governments did not do enough to improve hospitals and develop the workforce when they had the chance.
“You’re absolutely right,” he says, “and I can’t explain it.”
“I’ll own what we did, for good and not so good, but this Government needs to own what they’ve got here and now.”
Reti insists National would increase health spending if it gets back into government and that it is developing a wide-ranging plan for reforming the health sector. He refused to share details of his plan until closer to the election.
In the near term, Reti says a National-led government would not try to unwind the reforms that led to the merger of 20 district health boards into Te Whatu Ora, even though he believes the restructuring is failing.
“If we’re successful, I won’t undertake major structural change initially,” he says. “The sector’s tired.”
“For a period of time, we’ll just stabilise the sector, rebuild hope, rebuild the workforce, rebuild direction, just get the ship steady again with a clear path.”
Asked if he is committed to preserving a public health system accessible to all New Zealanders, Reti says: “I’ve seen what broken health systems look like, and the private model is not one I’d adhere to. We need to have a really strong public health service that is there when you need it. That safety need needs to be strong.”
“Yes, I do think it’s salvageable, absolutely.”
Alex Spence is a senior investigative journalist based in Auckland. Before joining the Herald, he spent 17 years in London where he worked for the Times, Politico, and BuzzFeed News.
HELP US INVESTIGATE
The Herald will continue reporting on the impact of the staffing crisis in New Zealand’s hospitals and we need your help. Do you have information on this topic? Have you or someone you know missed out on treatment because of capacity problems? Are you a hospital employee working under difficult conditions? Do you have documents that can help us shed light on these issues?
We want to speak to as many people as possible who have experience in the system, to ensure our reporting is thorough and accurate. You can reach Investigations Editor Alex Spence by email (alex.spence@nzme.co.nz), secure Signal messaging (0272358834), or post (The New Zealand Herald, Private Bag 92198, Victoria St West, Auckland CBD 1142.) We can’t reply to all submissions because of the volume we receive. We will not publish your name or identify you as a source unless you want us to.