Whangārei Hospital is down about half its house surgeons after international borders reopened and there’s a critical shortage of medical registrars.
Photo / Supplied
Whangārei Hospital is down about half its house surgeons after international borders reopened and there’s a critical shortage of medical registrars, a union representing resident medical officers says.
The New Zealand Resident Doctors’ Association (NZRDA)
said the roster of its members working in the medical and surgical units at Whangārei Hospital has “collapsed” as the workforce was down by between 40 per cent and 50 per cent.
“We’ve lost 18 house surgeons up until March this year and we’re critically short of medical registrars as well so Northland’s situation is critical in terms of a lack of cover for staff,” association national secretary Dr Deborah Powell said.
House surgeons are qualified doctors who practise general surgery under supervision in hospitals in the first four years after graduation.
Health NZ Te Tai Tokerau Health NZ Te Tai Tokerau employs 55 house officers while there are 15 vacancies at present.
General manager surgical and support services Mark McGinley said no surgeries have had to be postponed due to a shortage of house officers.
He said 94 registrars were employed across the various specialities and there are four vacancies at that level.
NZRDA represents resident medical officers which includes trainee interns, house surgeons, senior house officers and registrars. They held a meeting with Health NZ this week to negotiate a variation to the collective agreement.
Dr Powell said the collective agreement would help the Government to tackle the ‘leaky’ medical workforce pipeline.
Union proposals to increase New Zealand medical student numbers by 200 per year, employ medical students in their final year of training, and guarantee senior medical officer employment to doctors who complete their residency in New Zealand are being discussed with Health New Zealand.
Health Minister Andrew Little last week announced a suite of targeted measures to train more health workers domestically and bring more doctors and nurses into the country to help address immediate workforce pressures.
The package to boost the health workforce includes the establishment of a one-stop-shop for international recruitment within Health New Zealand, training more GPs and removing significant cost barriers for professional registration.
But Dr Powell said over reliance on doctors from the United Kingdom on working holidays has contributed to the current situation in Northland and elsewhere around the country.
“As soon as borders reopened, they left. That’s why the RDA has been critical of (Health Minister) Andrew Little’s position that the Government recruit people from overseas.
“Having said that, we need overseas workforce but we also have to train and retain local doctors so we are not in the crisis we are in at the moment. We are also losing doctors to Australia so it’s a double whammy for us,” Dr Powell said.
One of the main reasons resident doctors left their training programmes or moved overseas was due to concern about their future employment opportunities in New Zealand, she said.
“Compounding challenges within this workforce group at present are high levels of sick leave and additional out-of-hours duties, which require rest periods during daytime hours to ensure adequate recovery time.
“The driver of additional duties has been a sustained period of high inpatient activity levels within our hospitals,” he said.
Dr Powell said the establishment of Health NZ allowed the system to, for the first time, create long term job security for doctors on the pathway to specialist training.
“A recent survey of our members found that a guarantee of employment as a senior medical officer (SMO) upon completion of their vocational training would make a positive difference to their intention to remain in New Zealand for over 70 per cent of resident doctors.
“We have widespread issues with short staffing and multiple rosters across the country where only half the required number of doctors are working. Fixing the medical workforce pipeline is going to require a massive bolstering in the number of medical students, and then a range of initiatives to keep doctors in New Zealand,” she said.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/LEWVCDHD7DDNTACCALWBNPCJTU.jpg)
Photo / Supplied
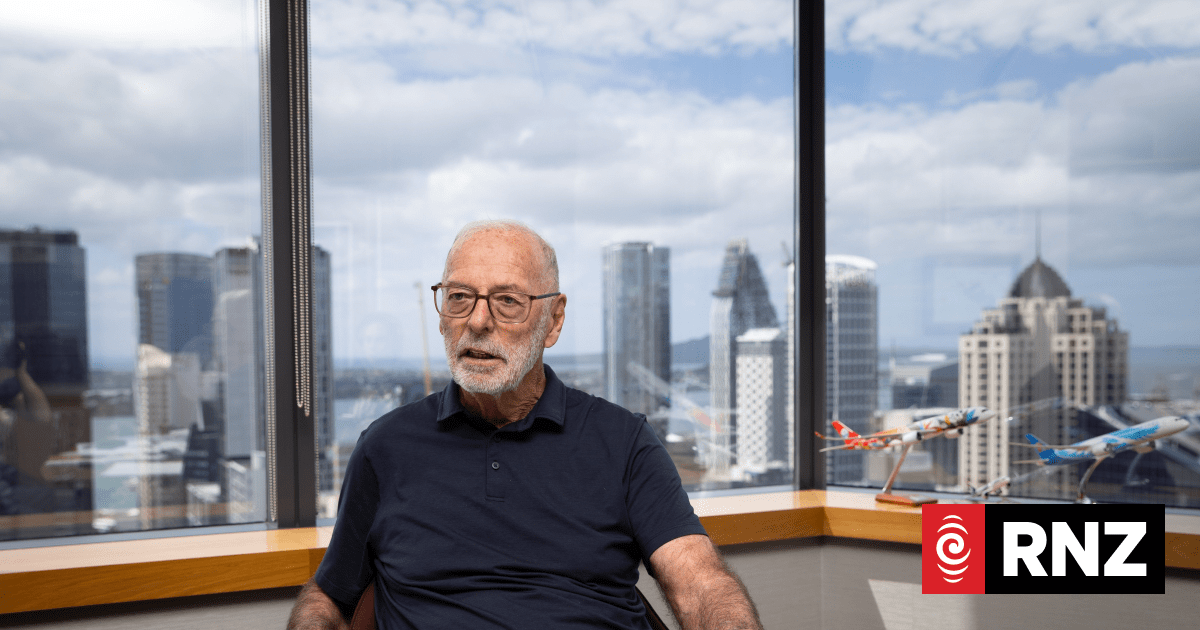
Dr Gary Payinda, an emergency medicine specialist at Whangārei Hospital, questioned the need to bring in doctors and nurses from abroad when meaningful initiatives could be undertaken to retain those who have been locally-trained.
Clinically, he said Northland’s public health service was in some significant distress with severe staffing problems and high sick leave among staff.
He said older and experienced nurses chose to retire early than continue at a “punishing” pace at the moment while younger ones were leaving for a much higher pay in Australia.
“We could easily increase the number of nurse training spots and bring training back to hospitals rather than just universities so they can get real life experience, and to pay them a reasonable stipend for them to remain in New Zealand,” Dr Payinda said.
The Government is streamlining and funding the system for international health workers, including doctors, to get their professional qualifications recognised in New Zealand.
For nurses, this includes funding of up to $10,000 each to complete and sit competence assessment programmes that can be needed to get registration in New Zealand.
/cloudfront-ap-southeast-2.images.arcpublishing.com/nzme/R2HBD5CDJAQ2VU4IS5WDD64A7M.jpg)
For doctors, there will be a six-month bridging programme to prepare them for working in New Zealand, including paying salaries during their six-week clinical induction courses and three-month training internships.
There will be a joint project with the Royal New Zealand College of General Practitioners to increase the number of GPs trained each year to 300 nationwide and to get more Māori and Pacific GPs.